Effects of an Integrated Rehabilitation Program on Fatigue in Patients with Pulmonary Tuberculosis
Keywords:
Pulmonary tuberculosis, Integrated program, Fatigue, Line applicationAbstract
Objective: This study aimed to assess the effect of a 6-weeks integrated rehabilitation program on fatigue in pulmonary tuberculosis patients.
Materials and Methods: Sixty-eight participants were diagnosed with pulmonary tuberculosis receiving antituberculosis drugs treated for 2 weeks or more. Participants were randomly into experimental and control groups with 34 participants each. The experimental group received usual care with an integrated rehabilitation program. The control group received the usual care with given the option to engage in activities to reduce their own fatigue. Fatigue symptoms were assessed with PFS-12 at baseline, at week 3 and week 6 and using the Repeated measure ANOVA for statistical analysis.
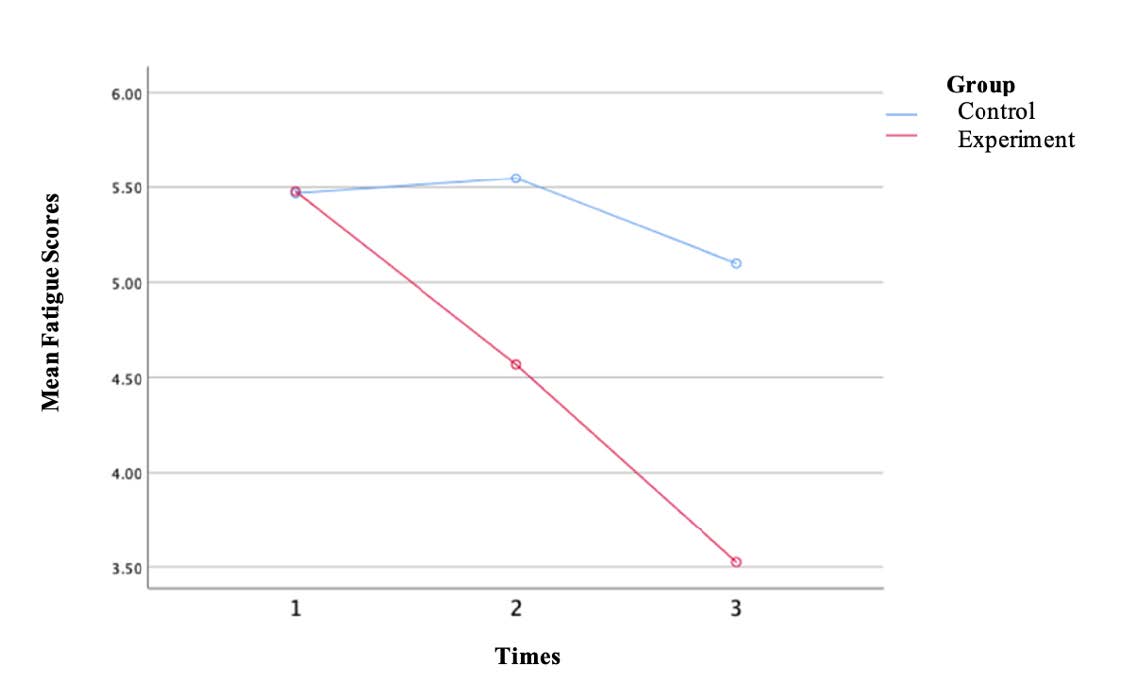
Results: The study found that the experimental group had a lower mean fatigue score at week 3 than at the pretest. At week 6, the mean fatigue score decreased significantly compared that at the pretest and compared to the control group with statistical significance (F = 9.698, p <.001), while no statistically significant differences were found in the control group (F = 1.687, p = .200)
Conclusions: The integrated rehabilitation program statistically and significantly reduced the levels of fatigue in pulmonary tuberculosis in 3-6 weeks.
Registration number: This study was registered at the Thai Clinical Trials Registry (TCTR20221202001).Keywords: Pulmonary tuberculosis; Integrated program; Fatigue; Line application
References
REFERENCES
Thedthong W, Puwarawuttipanich W, Saneha C, Rongrungruang Y. Factors predicting fatigue in pulmonary tuberculosis patients receiving anti-tuberculosis drugs. Siriraj Med J. 2021;73:167-73.
Sahebi L, Ansarin K, Maryam S, Monfaredan A, Sabbgh Jadid H. The factors associated with tuberculosis recurrence in the northwest and west of Iran. Malays J Med Sci. 2014;21:27-35.
Yang TY, Lin CL, Yao WC, Lio CF, Chiang WP, Lin K, et al. How mycobacterium tuberculosis infection could lead to the increasing risks of chronic fatigue syndrome and the potential immunological effects: A population-based retrospective cohort study. J Transl Med. 2022;20(1):99.
Schub TB, Lawrence PRMBBC. Tuberculosis in adults. Ipswich, Massachusetts: EBSCO Publishing; 2018.
Choi H, Park HA, Hyun IG, Kim J-H, Hwang Y-I, Jang SH, et al. Incidence and outcomes of adverse drug reactions to first-line anti-tuberculosis drugs and their effects on the quality of life: A multicenter prospective cohort study. Pharmacoepidemiol Drug Saf. 2022;31:1154-63.
Ting NCH, El-Turk N, Chou MSH, Dobler CC. Patient-perceived treatment burden of tuberculosis treatment. PLoS One. 2020;15:e0241124.
Li C-T, Chu K-H, Reiher B, Kienene T, Chien L-Y. Evaluation of health-related quality of life in patients with tuberculosis who completed treatment in Kiribati. J.Int. Med. Res. 2017;45:610-20.
Sarkar M, Srinivasa, Madabhavi I, Kumar K. Tuberculosis associated chronic obstructive pulmonary disease. Clin Respir J. 2017;11:285-95.
Amaral AFS, Coton S, Kato B, Tan WC, Studnicka M, Janson C, et al. Tuberculosis associates with both airflow obstruction and low lung function: BOLD results. Eur Respir J. 2015;46:1104.
Karimi P, Guantai A, Kigondu C, Ogaro T. Prevalence of adverse events of anti-tuberculosis drugs and their impact on adherence to treatment in Nairobi city county. Pharmaceutical Journal of Kenya. 2017;23:56-60.
World Health Organization. Global tuberculosis report 2020: Geneva; 2020.
Gilpin C, Korobitsyn A, Migliori GB, Raviglione MC, Weyer K. The world health organization standards for tuberculosis care and management. Eur Respir J. 2018;51.
Dodd M, Janson S, Facione N, Faucett J, Froelicher ES, Humphreys J, et al. Advancing the science of symptom management. J Adv Nurs. 2001;33:668-76.
Reeve BB, Stover AM, Alfano CM, Smith AW, Ballard-Barbash R, Bernstein L, et al. The Piper Fatigue Scale-12 (PFS-12): Psychometric findings and item reduction in a cohort of breast cancer survivors. Breast Cancer Res Treat. 2012;136:9-20.
Kronkasem A, Wattanakitkrileart D, Pongthavornkamol K, Kanoksin A. Fatigue experience, symptom management strategies, and functional status in patients with congestive heart failure. Nurs Sci J Thai. 2015;32:35-42.
Xu Z, Chen W, Li X. Effects of comprehensive nursing intervention combined with respiratory functional exercises on pulmonary function and self-care ability in patients with pulmonary tuberculosis: Results of a randomized trial. Ann Palliat Med. 2021;10:7543-50.
Akbar N, Nursasi AY. Pulmonary rehabilitation for people with pulmonary tuberculosis: A concept analysis based on walker and avant approach. Indian J Public Health Res Dev. 2019;10:1255-60.
Ahmed S, Sharma N, Patrikar S, Samiullah. Efficacy of early structured pulmonary rehabilitation program in pulmonary function, exercise capacity, and health-related quality of life for patients with post-tubercular sequelae: A pilot study. Med J Armed Forces India. 2022;78:164-9.
Visca D, Zampogna E, Sotgiu G, Centis R, Saderi L, D'Ambrosio L, et al. Pulmonary rehabilitation is effective in patients with tuberculosis pulmonary sequelae. Eur Respir J. 2019;53:e1802184.
Buono MJ, Lee NV, Miller PW. The relationship between exercise intensity and the sweat lactate excretion rate. J Physiol Sci. 2010;60:103-7.
Mulley C, Gebel K, Ding D. Walking: Connecting sustainable transport with health. Vol.9. Bingley: Emerald Publishing Limited; 2017.
Wipfli B, Landers D, Nagoshi C, Ringenbach S. An examination of serotonin and psychological variables in the relationship between exercise and mental health. Scand J Med Sci Sports. 2011;21:474-81.
Itagi ABH, Dipankar SP, Krishna Veni D, Yunus GY. Evaluation of spirometric measures and quality of sleep in tuberculosis patients and their non-tuberculosis family caregivers. Cureus. 2021;13:e17788.
Sukartini T, Hidayati L, Khoirunisa N. Knowledge, family and social support, self-efficacy and self-care behavior in pulmonary tuberculosis patients. J. keperawatan Soedirman. 2019;14:114-25.
Bao Y, Wang C, Xu H, Lai Y, Yan Y, Ma Y, et al. Effects of a mHealth intervention for pulmonary tuberculosis self-management based on the integrated theory of health behavior change: Randomized controlled trial. JMIR Public Health Surveill. 2022;8:e34277.
Aslam M, Safdar M, Khalid S, Sharmeen Z, Irfan T, Saher K. The effect of nutrition education on nutritional status of tuberculosis patients. Biomed J Sci Tech Res. 2021;33:25781-5.
Hu B, Ren G, Zhao L. Effect of health education combined with dietary guidance on nutritional indicator, immune level and quality of life of patients with pulmonary tuberculosis. Comput Math Methods Med. 2021;2021:e9463577.
DiStefano MJ, Schmidt H. mHealth for tuberculosis treatment adherence: A framework to guide ethical planning, implementation, and evaluation. Glob Health Sci Pract. 2016;4:211-21.
House JS. Social support and social structure. Sociol Forum. 1987;2:135-46.
Li X, Wang B, Tan D, Li M, Zhang D, Tang C, et al. Effectiveness of comprehensive social support interventions among elderly patients with tuberculosis in communities in China: A community-based trial. J Epidemiol Community Health. 2018;72:369-75.
Elfiyunai NN, Glorino Rumambo Pandin M. The role of nurses in providing social support in tuberculosis treatment: Literature review. Preprints. 2021.
Lekdamrongkul P, Pongthavornkamol K, Siritanaratkul N, Siripoon S, Jitnumsub P. The effects of concrete-objective information program on anxiety and functional status among lymphoma patients receiving chemotherapy. Nurs Sci J Thai. 2020;38:19-34.
Sribenjamas V, Tangkawanich T, Tunsupasawasdeekhul S, Linchareon A. The effect of symptom management program on fatigue and muscle strength in person living with HIV/AIDS. Journal of Nursing Science & Health. 2016;1:61-70.
Arslan S, Oztunc G. The effects of a walking exercise program on fatigue in the person with COPD. Rehabil Nurs. 2016;41:303-12.
Piper BF, Dibble SL, Dodd MJ, Weiss MC, Slaughter RE, Paul SM. The revised piper fatigue scale: Psychometric evaluation in women with breast cancer. Oncol Nurs Forum. 1998;25:677-84.
Thongsaman A, Jenpanich Wisutthiphan P, Samdangrit B. Symptom experiences, symptom management strategies and outcome related to adverse drug reactions of anti-TB drugs. Vajira Nursing. 2018;18:51-63.
Venes D. Taber's cyclopedic medical dictionary. New York: McGraw-Hill Education LLC; 2017.
Downloads
Published
How to Cite
License
Copyright (c) 2023 Siriraj Medical Journal

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Users are free to share, copy, and redistribute all articles published in the Siriraj Medical Journal (SMJ) in any medium or format as long as you follow the following terms:
- Attribution — You must give appropriate credit, provide a link to the material, and indicate if changes were made. You may do so in any reasonable manner, but not in any way that suggests the publisher endorses you or your use.
- NonCommercial — You may not use the material for commercial purposes.
- NoDerivatives — If you remix, transform, or build upon the material, you may not distribute the modified material.
- No additional restrictions — You may not apply legal terms or technological measures that legally restrict others from doing anything the license permits.






